Acute pulmonary hypertension
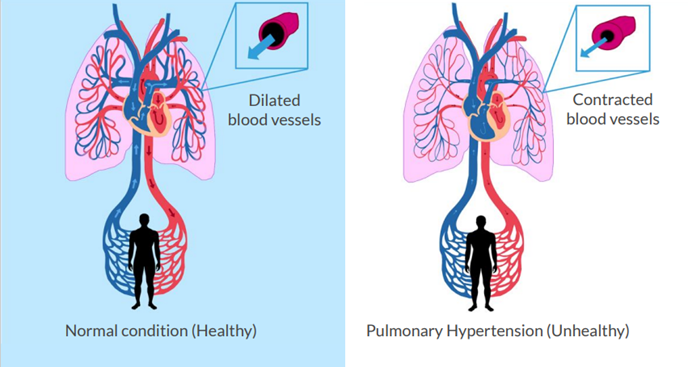
Acute pulmonary hypertension can be elicited by and complicate a variety of relatively common medical conditions such as blood clots in the lung, sepsis or as a complication to major surgery, especially after open cardiac surgery using heart-lung machines. The condition is often life-threatening because the right heart is a weak pump unable to pump blood through the pulmonary vessels at elevated pressures which ultimately results in right heart failure and death.
In association with surgery acute pulmonary hypertension is a well-known independent risk factor associated with mortality and bad outcome.
The mechanism is complex and include decreased functionality of the innermost layer of the lung blood vessels, the endothelium, resulting in decreased availability of the vessel dilating substance nitric oxide and increased levels of vasoconstricting substances e.g., substances produced by inflamed tissues. The overall result is an imbalance between vasoconstricting and vasorelaxant mechanisms. In many cases decreased oxygen tension in in diseased lungs also contributed by causing hypoxic vasoconstriction.
Market
The total incidence of acute pulmonary hypertension is difficult to estimate since it is frequently underdiagnosed and attempts to treat the condition in most cases begin only after serious complications have developed. One of the reasons for this is the lack of interest in diagnosing the condition is the lack of effective treatment and the relative complexity to measure the hemodynamic condition in the lung blood circulation. The optimal and most accurate way is to use pulmonary artery catheters which is an invasive technique that only some physicians can perform and although echocardiography could be used for rough estimate this method does not work in all patients. A consequence of the complexity of diagnosing and treating APH is that a standard disease codes for this condition has not yet been established.
However, despite the above-mentioned difficulties with diagnosis echocardiographic studies from general ICU care reveal that up to 30 percent of all intensive care treated patients have acute pulmonary hypertension and this has been shown to be an independent risk factor for bad outcome. Safe and effective treatment to prevent right-sided heart failure and death in acute pulmonary hypertension patients have long been sought for by intensive care doctors. The potential market for Supernitro in acute pulmonary hypertension is therefore vast and could eventually include all conditions with life-threatening acute pulmonary hypertension. The acute pulmonary hypertension market could be subdivided in different subgroups:
- Cardiac surgery
- Major surgeries (non cardiac)
- Pulmonary embolism (blood clots in the pulmonary circulation)
- Acute lung injury and/or acute respiratory distress syndrome often elicited by infections (e.g. Covid-19).
- Other conditions e.g., acute pulmonary hypertension in premature infants, or acute pulmonary hypertension in Bone cement implantation syndrome (BCIS) elicited by hip transplantation.
A conservative estimate is that acute pulmonary hypertension causes more than 100,000 deaths annually, only counting Europe, the United States and Japan. There is a significant potential for Attgeno to have its product, Supernitro, positioned as the primary treatment in this indication as Supernitro is lung selective, none or small systemic effects on the blood circulation, easy to use in the ICU setting and have a very benign safety profile.
Attgeno’s ambition is to gain market approval for Supernitro as a treatment for acute pulmonary hypertension regardless of the underlying cause. However, the explicit goal is to achieve a swift entry into the US market, and comprehensive analyses of clinical, regulatory and market possibilities have all pointed at addressing acute pulmonary hypertension elicited by cardiac surgery as a primary indication. acute pulmonary hypertension in the perioperative period during cardiac surgery is a key indication for Attgeno, as patient populations are clearly defined and there is a large need for more effective and simpler treatment.
Acute pulmonary hypertension in Cardiac surgery
Acute pulmonary hypertension in the perioperative period during cardiac surgery is a key indication for Attgeno, as patient populations are clearly defined and there is a large need for more effective and simpler treatment. It is a challenge for the surgical team to treat severe APH when diagnosed. Patients undergoing coronary artery bypass grafting (CABG) and/or heart valve surgery are at moderate to high risk of developing acute pulmonary hypertension.
Prevalence of pulmonary hypertension in patients admitted in ICU post operatively is used to identify the target population in this segment. It has been found from various sources that post-operative ICU admissions ranges from 3.5% to 14%.
With more complex cardiac surgery procedures, such as left ventricular assist device implantation, pulmonary thrombendarteriectomy or heart transplantation, pulmonary vasodilator treatment for acute pulmonary hypertension is usually required. In isolated CABG surgery acute pulmonary hypertension is less frequent but can become a huge problem in patients with already existing cardiopulmonary diseases, for example patients with any form of chronic pulmonary hypertension. In terms of target patient population, 25% of all cardiac surgery patients are at high risk of deleterious acute pulmonary hypertension, in most cases due to pre-existing pulmonary hypertension.
This means that annually almost 300,000 patients in the United States, the EU and Japan would benefit from Supernitro treatment to reduce the risk of death after cardiac surgery.
The difficulty of treating the condition is that most affected patients, while they have a high pressure in the pulmonary circulation, have low pressure in the systemic circulation whereby blood supply is threatened in the body’s vital organs. This establishes a vicious circle of acute pulmonary hypertension and right ventricular failure resulting in systemic hypotension, low cardiac output, diminished right coronary flow due to decreased pressure gradient and right ventricular ischemia.
To effectively treat the conditions, one must give drugs that dilate blood vessels in the lung but since drugs available today are not selective for lung vessels, blood vessels are also widened in the systemic circulation and risks that blood pressure in the body reaches critically low levels.
The logical treatment is to widen the constricted lung blood vessels and relieve the right heart, however when given intravenous vessel-dilating drugs the risk is that these will not only widen vessels in the lungs but also cause a general vasodilation in the systemic circulation and thereby dangerous drop in systemic blood pressure.
Chronic Pulmonary Hypertension
Various underlying diseases can induce this slow progressive vasoconstriction in the pulmonary circulation and lead to chronic changes in the lung blood vessels with small blood clots (thrombosis) and structural transformation of the blood vessels (vascular remodeling). Over time the lumen of vessels becomes increasingly narrow and resistance to blood flow increases and the vessels cannot dilate. This is called chronic pulmonary hypertension or often just pulmonary hypertension.
Some types of chronic pulmonary hypertension are treated with vasodilator drugs that can slow down the progression of the disease for some time and these treatments is usually continues for the rest of the patient’s life. However, despite treatments, the overall prognosis is poor and pulmonary hypertension gradually increases, eventually leading to right heart failure and death.
Patients with chronic pulmonary hypertension have shortness of breath, fatigue and dizziness, which are exacerbated by exercise. Symptoms are not specific for chronic pulmonary hypertension and diagnosis is usually delayed.
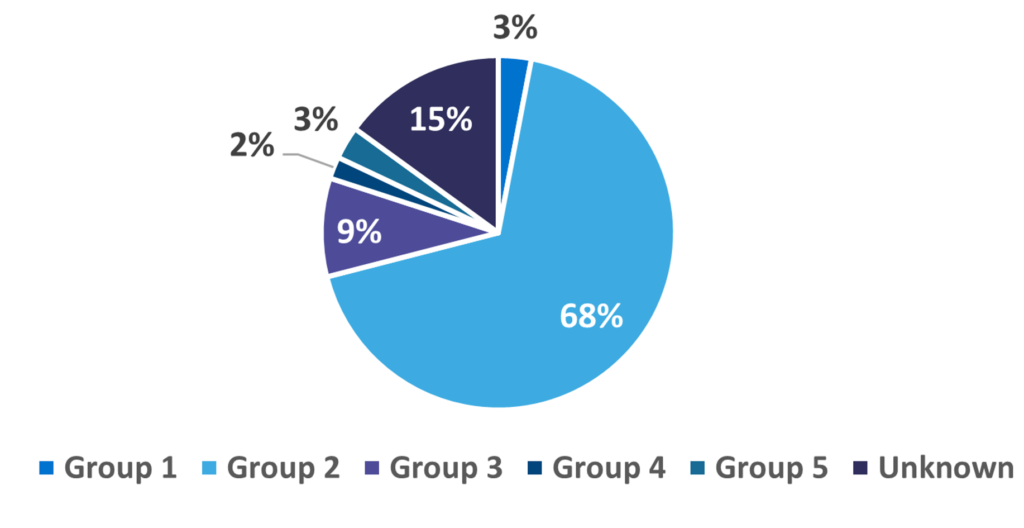
Based on the underlying cause WHO has dived Chronic Pulmonary hypertension is divided in five subgroups:
- Pulmonary arterial hypertension (PAH)
- Pulmonary hypertension due to left-sided heart disease (PH-LHD)
- Pulmonary hypertension related to lung disease and/or hypoxia
- Chronic thromboembolic pulmonary hypertension (CTEPH)
- Pulmonary hypertension related to unclear or multifactorial mechanisms
Patients with chronic pulmonary hypertension exert a major disease burden in all low-, middle- and high-income countries. Although chronic pulmonary hypertension has long been recognized to complicate many common diseases, especially left-sided heart disease and lung disease, most basic, translational and clinical scientists together with the pharmaceutical industry have, to date, focused predominantly on PAH and chronic thromboembolic pulmonary hypertension.
Market
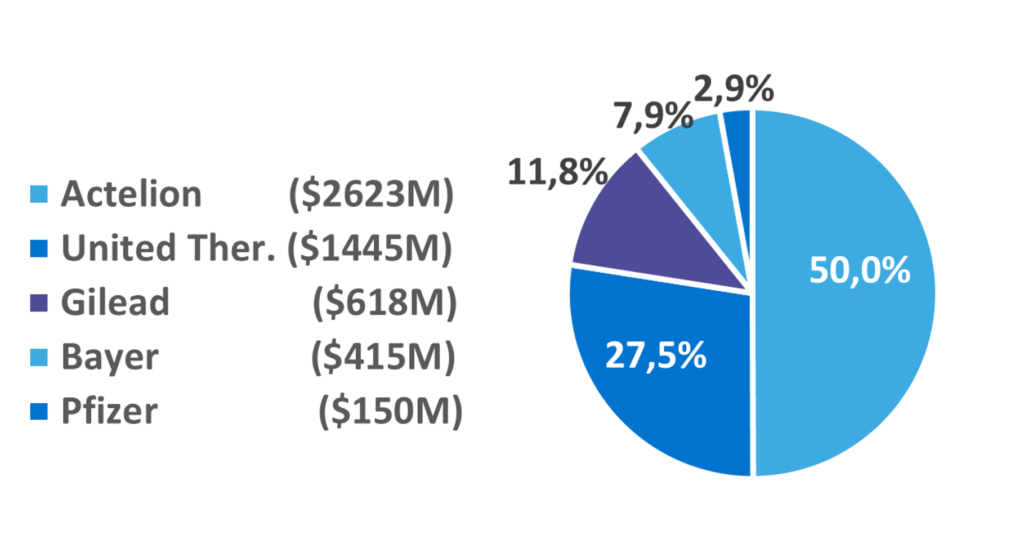
The total chronic pulmonary hypertension market in 2019 was USD26 billion in the seven major markets – the United States, Japan, Germany, France, Italy, Spain, the UK. Despite Groups 1 and 4 representing only about 5% of the total prevalence of chronic pulmonary hypertension, prescription in these groups constitutes almost the entire market.
It is evident that this is a huge potential market if effective treatments were to be approved for use in WHO Groups 2 and 3. There were almost 15 million cases in 2019 in the United States. Still, the ‘small’ level of prevalence in Group 4 generates a significant revenue stream for the companies who are operating there.
While to date, the true global burden of chronic pulmonary hypertension remains unknown, according to recent literature, it has certainly been underestimated. Chronic pulmonary hypertension should no longer be considered a rare disease and has marked its impact on world health for several salient reasons. First, chronic pulmonary hypertension is invariably associated with increased morbidity and mortality when occurring regardless of etiology. Second, the increasing age of populations worldwide is leading to a marked change in the distribution and groups of patients presenting with chronic pulmonary hypertension. Independent risk factors for development of CPH are older age, BMI, left ventricular dysfunction, chronic obstructive pulmonary disease (COPD) and systemic hypertension. Using echocardiography to assess chronic pulmonary hypertension, the ERGO Rotterdam study showed a prevalence of 2.6% of the general population.
